|
Case Report
A case report of a testicular spermatocytic tumor in an 89-year-old patient
1 Urology Department, Transplant Kidney andRobotic Surgery, ARNAS Giuseppe Brotzu, San Michele Hospital, Cagliari, Italy
2 Department ASL, Sulcis, Urology, Sirai Hospital, Carbonia, Italy
3 Pathology Department, ARNAS Giuseppe Brotzu, San Michele Hospital, Cagliari, Italy
Address correspondence to:
Riccardo Farci
Urology Department, ASL Sulcis, Sirai Hospital, Via Ospedale, 09013 Carbonia,
Italy
Message to Corresponding Author
Article ID: 100055Z15AS2025
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Solinas A, Farci R, Bianco P, Onnis D. A case report of a testicular spermatocytic tumor in an 89-year-old patient. J Case Rep Images Urol 2025;10(2):29–32.ABSTRACT
Spermatocytic tumor is a very rare clinical entity representing 1% of testicular tumors affecting elderly males with a men age of 52–59 years. It lacks features associated with tumors derived from germ-cell neoplasia in situ (GCNIS) including cryptorchidism and racial or ethnic predisposition. We present the case of an 89-year-old man with spermatocytic tumor admitted in the unit of urology with right-sided testicular swelling. In this paper we discuss the histopathology and ultrasound features of this testicular tumor.
Keywords: Germ cell tumors, Spermatocytic tumor, Testis
Introduction
Spermatocytic tumor was first reported by Masson in 1946 and termed as “Spermatocytic seminoma” due to false belief of its origin from germ-cell neoplasia in situ (GCNIS) and renamed as “Spermatocytic tumor” in the WHO 2016 classification. It represents only 1% to 2% of testicular germ cell tumors and occurs with about 1/100th the frequency of seminoma [1]. Unlike other types of germ cell tumor, it occurs only in the testis, except of one unique case in a dysgenetic gonad [2], slightly more frequent on the right side and is bilateral in up to 9% of cases. Also, unlike almost all other germ cell tumors that occur in post-pubertal patients, spermatocytic tumor is not associated to cryptorchidism, GCNIS, or other types of germ cell tumor. It occurs as a pure lesion, except in rare cases in which it is associated with sarcoma. In literature there are some cases described as “anaplastic” variant and spermatocytic tumor with sarcoma. The “anaplastic” variant was described in 1996 and since then only isolated cases have been reported [3],[4], while the association with sarcoma is well documented in several cases [5],[6] and these tumors are distinctively high grade with potential capability to metastasize. Spermatocytic tumor is characterized by a slow progression, an early stage at the time of diagnosis, and the absence of metastases. Most patients with spermatocytic tumor are older than those with other types of testicular germ cell tumors with an average of 40 years for patients with seminoma. Nevertheless spermatocytic tumor with sarcomatous differentiation has a poor prognosis, a high risk of metastasis of the sarcomatous component to the lungs, a high mortality rate and highly resistant to treatments [7]. We present the case of spermatocytic tumor in an 89-year-old man who was admitted in our department for a right-sided testicular mass.
Case Report
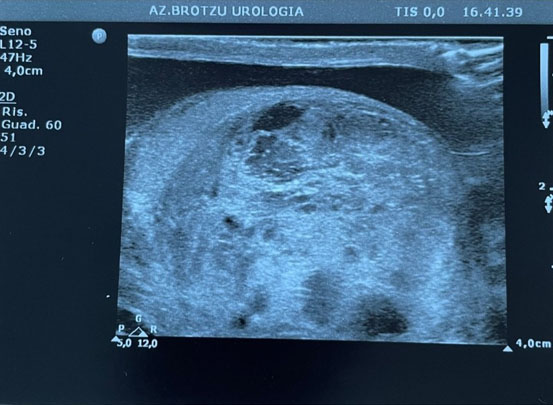
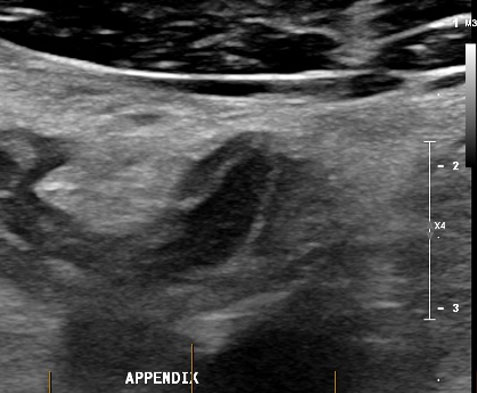
An 89-year-old man was admitted to the Department of Urology for testicular swelling and tenderness for five months with associated comorbidities of urolithiasis, atrial fibrillation in oral anticoagulant therapy, pleuritis, and hypertension. His testicular tumor markers [alpha-fetoprotein (AFP), beta-human chorionic gonadotropin (β-hCG), and lactate dehydrogenase (LDH)] were normal. A physical examination revealed a right testicular mass with normal skin and left testicle without abnormalities. Scrotal ultrasound (Figure 1) showed the presence of a large (4.16 × 2.26 cm) tumor with circular dichroism (CD) signal occupying the whole right testicle with heterogeneous echogenicity and smaller anechoic cystic components with minimal presence of normal testicular tissue. The left testicle was normal. A total-body computed tomography (CT) scan was performed and showed no signs of metastatic disease or lymphadenopathy. On suspicion of testicular cancer a right-sided radical orchiectomy was performed. Surgery was uncomplicated and he was discharged the day after the surgery. The patient had a close 12 month follow-up without need of any therapy and was in good condition 22 months after surgery.
Histological examination
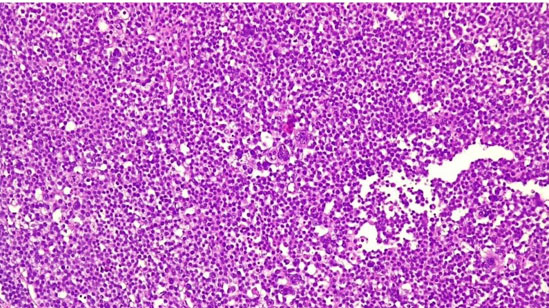
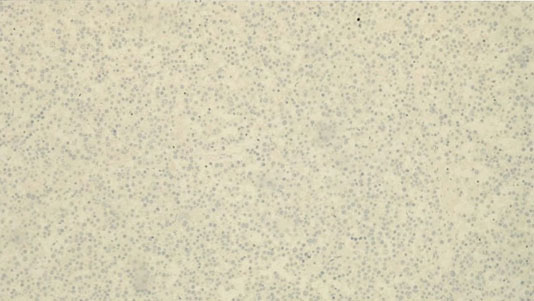
Grossly the tumor was well circumscribed with a nodular appearance, and a maximum diameter of 41 mm, on cut showed zones of fleshy, white to tan tissue, mucoid, and gelatinous change without paratesticular extension. Microscopically the tumor showed a polymorphous population of cells (Figure 2) that consists of three major types: a small, lymphocyte-like cell, an intermediate-sized cell, and giant cell, some of which were multinucleated. The borders between cells, in contrast with seminoma, were indistinct. No prominent lymphocyte infiltrates were found, neither was a GCNIS. No evidence of infiltration of rete testis or paratesticular structures was found. Most immunohistochemical markers of germ cell including OCT3/4 (Figure 3), CD30, Glypican-3, beta-hCG, and PLAP were negative as well as lymphoid markers (CD20, CD79a, Bcl-2, Bcl-6, c-Myc, MUM-1, and PAX-5). On the contrary CD 117 was focally positive. Based on immunohistochemistry as well as morphology the tumor was classified as a spermatocytic tumor.
Discussion
Spermatocytic tumor is a rare germ cell tumor, representing less than 2% of testicular cancers. It is derived from post-pubertal-type germ cells that, until 2016, were called spermatocytic seminoma due to a false belief in its origin from germ cell neoplasia in situ [8]. In 2016 the WHO changed the name of spermatocytic seminoma to spermatocytic tumor because of particular clinical-pathologic features when compared with other forms of germ cell tumors [9]. The spermatocytic tumor usually occurs in an older age group but it is not a prerequisite for the diagnosis, as this entity has been reported in patient as young as 19 years. Spermatocytic tumor is not known to occur in extratesticular location and orchiectomy is curative [9]. Sarcomatous transformation and metastasis are very rare and usually this neoplasm follows an indolent course. The eventuality of sarcomatous transformation raises the question whether surgery should be supplemented by adjuvant treatment. However, the experience has been limited to few case reports and small series. The association of spermatocytic tumor with cryptorchidism is rare as evidenced by only two documented cases in literature so far [10].
Conclusion
Although relatively rare and usually indolent, spermatocytic tumor can be present in anaplastic variant or in association with sarcoma, for this reason we recall the importance of its diagnosis and treatment.
REFERENCES
1.
Patel PM, Patel HD, Koehne EL, Doshi C, Belshoff A, Seffren CM, et al. Contemporary trends in presentation and management of spermatocytic seminoma. Urology 2020;146:177–82. [CrossRef]
[Pubmed]

2.
Gru AA, Williams ES, Cao D. Mixed gonadal germ cell tumor composed of a spermatocytic tumor-like component and germinoma arising in gonadoblastoma in a phenotypic woman with a 46, XX peripheral karyotype: Report of the first case. Am J Surg Pathol 2017;41(9):1290–97. [CrossRef]
[Pubmed]

3.
Albores-Saavedra J, Huffman H, Alvarado-Cabrero I, Ayala AG. Anaplastic variant of spermatocytic seminoma. Hum Pathol 1996;27(7):650–5. [CrossRef]
[Pubmed]

4.
Dundr P, Pesl M, Povýsil C, Prokopová P, Pavlík I, Soukup V, et al. Anaplastic variant of spermatocytic seminoma. Pathol Res Pract 2007;203(8):621–4. [CrossRef]
[Pubmed]

5.
Stueck AE, Grantmyre JE, Wood LA, Wang C, Merrimen J. Spermatocytic tumor with sarcoma: A rare testicular neoplasm. Int J Surg Pathol 2017;25(6):559–62. [CrossRef]
[Pubmed]

6.
Wetherell D, Lawrentschuk N, Gyomber D. Spermatocytic seminoma with sarcoma: An indication for adjuvant chemotherapy in localized disease. Korean J Urol 2013;54(12):884–7. [CrossRef]
[Pubmed]

7.
Secondino S, Viglio A, Neri G, Galli G, Faverio C, Mascaro F, et al. Spermatocytic tumor: A review. Int J Mol Sci 2023;24(11):9529. [CrossRef]
[Pubmed]

8.
Moch H, Cubilla AL, Humphrey PA, Reuter VE, Ulbright TM. The 2016 WHO classification of tumours of the urinary system and male genital organs–Part A: Renal, penile, and testicular tumours. Eur Urol 2016;70(1):93–105. [CrossRef]
[Pubmed]

9.
Hu R, Ulbright TM, Young RH. Spermatocytic seminoma: A report of 85 cases emphasizing its morphologic spectrum including some aspects not widely known. Am J Surg Pathol 2019;43(1):1–11. [CrossRef]
[Pubmed]

10.
Stevens MJ, Gildersleve J, Jameson CF, Horwich A. Spermatocytic seminoma in a maldescended testis. Br J Urol 1993;72(5 Pt 1):657–9. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Andrea Solinas - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Riccardo Farci - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Paola Bianco - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Daniela Onnis - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2025 Andrea Solinas et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.