|
Case Report
Renal infarction caused by fibromuscular dysplasia
1 Rentek HD Center, İstanbul, Turkey
Address correspondence to:
Gurkan Yurteri
Rentek HD Merkezi, İstanbul,
Turkey
Message to Corresponding Author
Article ID: 100031Z15GY2023
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Yurteri G. Renal infarction caused by fibromuscular dysplasia. J Case Rep Images Urol 2023;8(1):14–16.ABSTRACT
Introduction: Fibromuscular dysplasia (FMD) is an atherosclerotic/non-inflammatory disease, usually involving the renal and internal carotid arteries. Renal infarction is a rare condition that can present with flank pain and can be caused by FMD.
Case Report: A 49-year-old female patient was admitted to the emergency department with complaints of flank pain, fever, nausea, vomiting, and chills. Her blood pressure was normal. Abdominal examination showed right costovertebral tenderness. Laboratory assessment showed hematuria, leukocytosis, increased C-reactive protein (CRP), and increased lactate dehydrogenase (LDH). Nephrolithiasis was strongly considered a cause of pain because of the nature of the pain and the presence of hematuria. The urinary system ultrasound was normal. On the computed tomography (CT), in contrastenhanced sections, an infarct area was detected in the lower pole of the right kidney. In renal angiography, severe focal stenosis was seen in the polar renal artery, and angioplasty was made.
Conclusion: Renal infarction can be caused by FMD and may be misdiagnosed as renal colic.
Keywords: Fever, Flank pain, Fibromuscular dysplasia, Renal infarction
Introduction
Fibromuscular dysplasia (FMD) is a disease that causes stenosis, aneurysm, dissection, and occlusion in the arteries. It is not due to atherosclerosis or inflammation and usually involves the renal and internal carotid arteries [1]. Renal infarction is a rare condition; this diagnosis is made only in 0.007% of patients in the emergency room [2]. Renal infarction is often caused by atherosclerosis and vasculitis, while it is rarely caused by fibromuscular dysplasia. Renal infarction is challenging to diagnose because it presents with non-specific abdominal pain [3]. The average time until the diagnosis of renal infarction after admission is two days [4]. In this report, we present a case of flank pain presenting to the emergency department (ED) and discuss the evaluation and overall treatment of renal infarction due to FMD.
Case Report
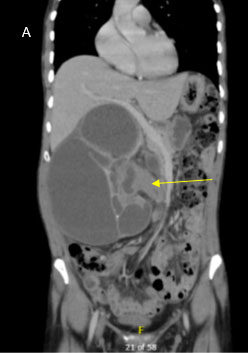
A 49-year-old female patient without a known disease was admitted to the ED with flank pain, fever, nausea, vomiting, and chills. She did not have a history of drug use and her family history was normal. The pain was colicky and severe. Her fever was 37.4–38°C, and her blood pressure was normal. Except for right costovertebral tenderness, other system examinations were normal. Her laboratory assessment showed hematuria, leukocytosis 18.1 × 109/L, increased CRP: 126.5 mg/L (<5 mg/L), and normal kidney and liver function tests [blood urea nitrogen (BUN) 20 mg/dL, creatinine 0.6 g/dL]. Nephrolithiasis was strongly considered a cause of pain but ultrasonography was found to be normal. For differential diagnosis LDH was measured and found to be 1422.3 U/L (135–225). In contrast-enhanced CT sections, an infarct area was detected in the lower pole of the right kidney (Figure 1). Enoxaparin sodium 2×0.4 mL SC was administered as an anticoagulant. Tests were negative to exclude possible vasculitis (anti-double stranded DNA, antineutrophilic cytoplasmic antibody, anticardiolipin IgG, IgM, Venereal Disease Research Laboratory Tests).
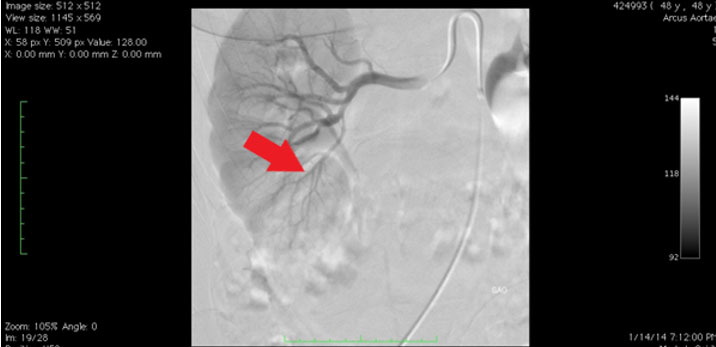
The patient underwent renal angiography two days later. Focal severe stenosis was detected in the polar renal artery at the postero-inferior level (Figure 2). Then, balloon dilatation was performed.
On the third day of hospitalization, the patient no longer needed analgesics. On the fourth day, LDH and CRP values were normal. Her hematuria disappeared, and antiaggregant (acetylsalicylic acid 300 mg) 1×1 treatment was started. She is now being followed up in the nephrology out-patient clinic with normal glomerular filtration rate.
'
Discussion
The incidence of renal infarction is very low. In a study conducted on emergency room patients, the incidence was 0.004–0.007% [5],[6]. Its frequency is 0.14% in autopsy sets [7]. Early diagnosis is difficult due to non-specific findings. The most common results in renal infarction patients are abdominal pain (53%), flank pain (50%), acute hypertension (48%), nausea (16.9%), vomiting (13%), and fever (10%) [8]. These findings can be seen in nephrolithiasis and pyelonephritis. High LDH is seen in 90.5% of renal infarctions [9]. In our case, all clinical and laboratory findings were detected except HT.
In 64% of the cases in the literature, the leading cause was a thromboembolic event due to atrial fibrillation [10]. It can also be seen in coagulation disorders, vasculitis, traumas, and diseases that disrupt the vascular structure, such as Ehlers–Danlos syndrome, Marfan syndrome, and FMD [6]. In the biochemical and radio diagnostic examinations done on our patient, no reason other than FMD was found. In FMD, the fibromuscular band folds and aneurysm enlargements may cause thrombi formation due to platelet activation [11].
Renal artery pathologies are seen bilaterally at 35–50% [12]. In our case, the left kidney vascular structure was normal.
In the past, selective renal arterial angiography was the gold standard for diagnosis. Angiographic classification includes the multifocal type, with multiple stenosis, and the “string-of-beads” appearance that is related to medial FMD, and tubular and focal types, which are not clearly related to specific histological lesions. Today, non-invasive methods such as Doppler sonography, CT scans, and magnetic resonance imaging (MRI) scans are performed [13].
The main goal of treatment is to prevent persistent parenchymal loss and control hypertension (HT). Since our patient had a loss of renal parenchyma, renal angiography and angioplasty were performed for diagnosis and treatment. Fibromuscular dysplasia patients may present with renal colic because of renal ischemia, as in our case. However, the absence of hypertension and its course with RI is a rare condition in FMD [14],[15].
Conclusion
In conclusion, FMD should be considered in the etiology of renal infarction in patients even if they are normotensive and presenting with the symptoms of renal colic.
REFERENCES
1.
Olin JW, Sealove BA. Diagnosis, management, and future developments of fibromuscular dysplasia. J Vasc Surg 2011;53(3):826–36.e1. [CrossRef]
[Pubmed]

2.
Rana MN, Al-Kindi SG. Prevalence and manifestations of diagnosed fibromuscular dysplasia by sex and race: Analysis of >4500 FMD cases in the United States. Heart Lung 2021;50(1):168–73. [CrossRef]
[Pubmed]

3.
Touzé E, Oppenheim C, Trystram D, et al. Fibromuscular dysplasia of cervical and intracranial arteries. Int J Stroke 2010;5(4):296–305. [CrossRef]
[Pubmed]

4.
Persu A, Touzé E, Mousseaux E, Barral X, Joffre F, Plouin PF. Diagnosis and management of fibromuscular dysplasia: An expert consensus. Eur J Clin Invest 2012;42(3):338–47. [CrossRef]
[Pubmed]

5.
Huang CC, Lo HC, Huang HH, et al. ED presentations of acute renal infarction. Am J Emerg Med 2007;25(2):164–9. [CrossRef]
[Pubmed]

6.
Domanovits H, Paulis M, Nikfardjam M, et al. Acute renal infarction. Clinical characteristics of 17 patients. Medicine (Baltimore) 1999;78(6):386–94. [CrossRef]
[Pubmed]

8.
Bourgault M, Grimbert P, Verret C, et al. Acute renal infarction: A case series. Clin J Am Soc Nephrol 2013;8(3):392–8. [CrossRef]
[Pubmed]

9.
Hazanov N, Somin M, Attali M, et al. Acute renal embolism. Forty-four cases of renal infarction in patients with atrial fibrillation. Medicine (Baltimore) 2004;83(5):292–9. [CrossRef]
[Pubmed]

10.
Antopolsky M, Simanovsky N, Stalnikowicz R, Salameh S, Hiller N. Renal infarction in the ED: 10-year experience and review of the literature. Am J Emerg Med 2012;30(7):1055–60. [CrossRef]
[Pubmed]

11.
Domanovits H, Paulis M, Nikfardjam M, et al. Acute renal infarction. Clinical characteristics of 17 patients. Medicine (Baltimore) 1999;78(6):386–94. [CrossRef]
[Pubmed]

12.
Olin JW. Recognizing and managing fibromuscular dysplasia. Cleve Clin J Med 2007;74(4):273–4, 277–82. [CrossRef]
[Pubmed]

13.
Andreoni KA, Weeks SM, Gerber DA, et al. Incidence of donor renal fibromuscular dysplasia: Does it justify routine angiography? Transplantation 2002;73(7):1112–6. [CrossRef]
[Pubmed]

14.
Slovut DP, Olin JW. Fibromuscular dysplasia. N Engl J Med 2004;350(18):1862–71. [CrossRef]
[Pubmed]

15.
Shlomai G, Belkin A, Goitein O, Portnoy O, Grossman E. A normotensive patient with fibromuscular dysplasia presenting as unilateral renal infarction. Isr Med Assoc J 2013;15(5):258–9.
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Gurkan Yurteri - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthor declares no conflict of interest.
Copyright© 2023 Gurkan Yurteri et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.