|
Case Report
A case of hydrocele repair: Legal aspect of consenting and post-operative complication
1 Clinical Fellow, Urology, The Mid and South Essex NHS Foundation Trust, Southend-on-Sea, Essex, United Kingdom
Address correspondence to:
Divya Bheenick
47 Chartwell Plaza, 9 Southchurch Road, Southend-on-Sea, Essex SS1 2BQ,
United Kingdom
Message to Corresponding Author
Article ID: 100026Z15DB2022
Access full text article on other devices
Access PDF of article on other devices

How to cite this article
Bheenick D. A case of hydrocele repair: Legal aspect of consenting and post-operative complication. J Case Rep Images Urol 2022;7(2):5–10.ABSTRACT
Introduction: The duties of a doctor are not only limited to providing medical treatment or surgical interventions to patients but also involve appropriate communication with them. Providing adequate information, addressing patients’ concerns, and respecting their decision making is all part of a doctors’ work ethics. The case describes a patient who had a hydrocele repair and developed early post-operative complications. The concern raised is whether adequate information regarding the procedure was given to the patient.
Case Report: A 45-year-old medically healthy man was referred to the urology department by his general practitioner for an enlarging right-sided hydrocele. The main reason for seeking treatment was cosmetic. Due to the coronavirus (COVID-19) pandemic, he had a non-face-to-face urology clinic appointment only a few months later. After having discussed the various management options with the urologist, he opted to have a hydrocelectomy. On the day of the surgery, several months later, the operating surgeon consented the patient whereby he again explained the procedure and the associated risks. The surgery itself was uneventful, unfortunately, he developed early post-operative complications. He presented with increasing scrotal pain and swelling, features suggestive of an infected hematoma. He was managed conservatively with oral analgesia and antibiotics after which his symptoms improved. However, a Doppler ultrasound scan performed two weeks later, showed an avascular right testicle. He was immediately admitted to the hospital and was taken to theater for a scrotal orchidectomy. The outcome of the procedure was unexpected and even more undesirable cosmetically. The patient was dissatisfied and eventually lodged a formal complaint in the Patient Advice and Liaison Service (PALS).
Conclusion: Post-operative complications can occur. However, providing patients with timely and adequate information ensures that the standard of care is met.
Keywords: Complication, Hydrocele surgery, Orchidectomy
Introduction
Amidst the ongoing COVID-19 pandemic, clinicians have witnessed dramatic changes in the provision of medical services. Consequently, many clinical consultations are now being performed remotely rather than face-to-face. Despite this major change, it is essential for medical practitioners to abide to the appropriate standard of care given to patients. It is crucial that patients are involved in their care; information regarding the condition, the need for treatment, the various management options, and the benefits or risks involved with each treatment must be discussed thoroughly. Moreover, individual needs and particular concerns of patients must be addressed [1].
As in this case presentation, a man in his forties presented with an increasingly bothersome and cosmetically unacceptable right sided hydrocele. He underwent a hydrocele repair that unfortunately resulted in the loss of his right-sided testicle due to post-operative complications. He was very upset with the outcome of the surgery. The complications of the procedure were discussed with him but the timing thereof was not ideal. The question that arises is whether the standard of care was met in this patient’s case?
According to medical evidence, the risk of testicular injury is very low at 0.3% after a hydrocelectomy [2]. However, as stated in March 2015 by the UK Supreme Court (Montgomery v Lanarkshire Health Board), it is the doctor’s duty to provide all relevant information involved in the treatment of a patient. It is the informed patient who then determines which intervention, if any, he or she would like to undergo [3]. This highlights, the importance of an appropriate initial consultation and informed consent before any intervention or treatment, allowing adequate time for patients to weigh the risks and benefits of each available option.
Case Report
A 45-year-old male patient was referred to the urology department by his General Practitioner (GP) for right sided scrotal swelling. He was reviewed by the GP in December 2019 and had an ultrasound scan of the scrotum showing a 9 cm right sided hydrocele with no other underlying testicular pathology. He was referred to the urology team in January 2020. Due to the COVID-19 pandemic, he received a non-face-to-face urology appointment only in February 2021.
During the consultation, he described that the right-sided scrotal swelling had been present for years and increasing gradually in size. However, over the last year, the swelling had increased significantly to the size of a tennis ball. It caused severe discomfort especially when he moved about due to friction with his clothing. It was cosmetically displeasing and socially embarrassing at times.
The patient’s medical history included gout for which he was not taking any medication and a tonsillectomy. There were no known drug allergies. He was a non-smoker and consumed around 10 units of alcohol per week. He lived with his wife and two children.
The consultant explained to the patient that a hydrocele is not a sinister disease and any form of treatment would only improve his quality of life.
The management options and associated risks were discussed. The choices were either to monitor the swelling only or to have a surgical intervention, namely aspiration or repair of the hydrocele. With aspiration of the hydrocele, the recurrence rate was high and complications such as hematoma formation and infection could occur. Alternatively, a hydrocelectomy had a higher chance of repairing the defect, but risks such as swelling of the scrotum, pain, bruising, bleeding into the scrotum were not uncommon. Other associated complications with the surgery were scrotal abscess formation needing further surgery and drain insertion or chronic scrotal pain. A small percentage of recurrence of the hydrocele was also possible. It is noted that during this consultation the risk of testicular injury was not mentioned.
The patient decided to proceed with a hydrocele repair. A British Association of Urological Society (BAUS) information leaflet for the procedure was sent to him and he was added to the waiting list for surgery.
On 20 August 2021, he attended the hospital for his intervention as a day case procedure. He was consented by the operating surgeon who again explained the complications associated with the surgery such as bleeding, scrotal hematoma requiring evacuation, wound infection, recurrence of the hydrocele, chronic scrotal pain, testicular atrophy, and in rare cases loss of testis.
The surgery was uneventful. The intra-operative findings were a thickened tunica vaginalis, an inflamed right-sided epididymis and 350 mL of straw-colored fluid.
There were no immediate post-operative complications and the patient was discharged after review by the surgeon. No further follow-up was arranged.
Six days after the surgery the patient presented to the Accident and Emergency (A&E) department with right scrotal swelling and a constant throbbing pain. He rated the pain as 9 over 10 on movement and 2 over 10 when he laid still. On occasion there was some blood spotting on his underpants. There were no urinary symptoms such dysuria or hematuria. He was otherwise systemically well.
He was referred to the urology team for further assessment. On examination, he was clinically stable. The vital signs revealed a pulse rate of 89/min, a blood pressure of 128/80 mmHg, a temperature of 37.5°C, and a respiratory rate of 18/min. Local examination revealed a right-sided scrotal swelling with induration of the skin. No obvious fluctuant swelling was present. The spermatic cord was thickened and tender on palpation.
A wound swab was taken and sent for microscopy, culture and sensitivity testing. A urine analysis did not reveal any abnormality. No blood tests were done.
He was managed conservatively for a likely epididymo-orchitis with analgesia and oral antibiotics, namely, co-amoxiclav 625 mg three times a day (TDS) for 7 days. An urgent Doppler ultrasound scan of the testis was arranged as an outpatient. The investigation was requested to rule out any scrotal abscess or testicular injury.
When he was reviewed a week later by the urology team, the patient reported a marked improvement in his symptoms. The pain had completely resolved. On examination, there was only minimal swelling of the right scrotum and the overlying skin was normal. On palpation, a hard lump separate from the testis was felt but was not tender.
Clinically, it was likely to be an organized blood clot and the infective process appeared to be resolving. The patient was reassured and sent home.
The patient had a blood test done to check his inflammatory markers on the same day of the outpatient ultrasound scan. Baseline serum hematology and biochemistry revealed normal counts with a white blood cell of 10.1 × 109/L, a hemoglobin of 145 g/L, a creatinine of 83 umol/L and an estimated glomerular filtration rate of more than 60 mL/min/1.73 m2.
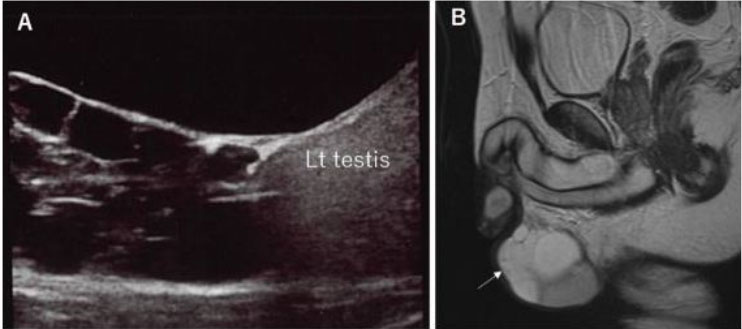
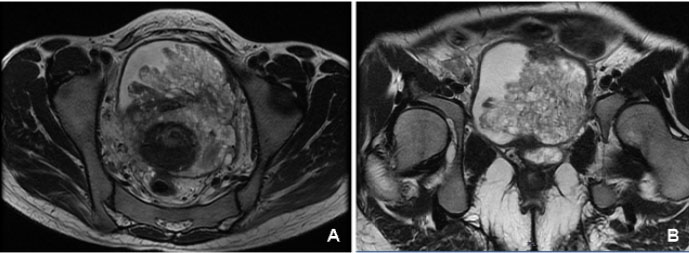
The Doppler ultrasound scan performed 2 weeks after the initial review described the right testicle as appearing diffusely hypoechoic with no presence of internal vasculature. The right scrotum also had a collection with internal septum suggestive of an infected hematoma (Figure 1). The left testis and epididymis had normal echotexture and vasculature. The ultrasound scan therefore showed radiological features of an avascular right sided testicle (Figure 2).
The likely differential diagnosis of ipsilateral scrotal swelling and pain one week after a hydrocelectomy includes hematoma, wound infection, scrotal abscess, or epididymo-orchitis [4]. An inguinal hernia although unrelated to the surgery should also be considered for unilateral scrotal swellings.
Clinically the swollen scrotum, indurated skin and mild serosanguinous discharge from the wound can be expected findings after such an operation. However, when the symptoms and signs of scrotal swelling and pain become worse, an infective process must be ruled out, as was the patient’s case. On the second review, when his clinical symptoms improved, it was assumed that he was responding to the antibiotics. Even the inflammatory markers were within a normal range.
However, when diagnosing scrotal pathologies especially after a surgery, physical examination, although important, is not completely reliable. The most effective way of ruling out other scrotal and testicular differential diagnoses would be with an ultrasound scan [5]. As in this case, the scan confirmed an infected scrotal hematoma but also showed an avascular testicle.
After the ultrasound scan, the patient was immediately sent back to the A&E department by the radiological team. He was assessed by the A&E doctors and was referred back to the urology team who admitted him. Blood and urine investigations were performed urgently. He was kept fasting overnight. Supportive treatment such as analgesia, intravenous fluids and antibiotics were initiated.
The on-call urology consultant reviewed him the next day. Management options namely, conservative treatment or expedited surgery were discussed with the patient. Conservative management would include treating the infection with antibiotics and removing the testicle at a later date. The risks involved would be ongoing pain secondary to the infection and testicular atrophy. On the other hand, an expedited surgery implied scrotal exploration and possible right sided orchidectomy during this admission itself. The patient opted for the latter.
Arrangement was made for him to have the procedure later that same day. Intra-operative findings were consistent with the ultrasound scan. The previous surgical wound had healed well. The right scrotum was mildly swollen with ongoing cellulitis of the scrotal wall. A scrotal hematoma was evacuated revealing a necrotic right testicle which was ligated and removed (Figure 3). A corrugated surgical drain was inserted in the scrotum.
The post-operative recovery was uneventful and the patient was discharged home the next day with oral co-amoxiclav for another 10 days. Follow-up with the benign urology nurse specialist was arranged to assess the wound healing and drain output. The drain was eventually removed after 48 hours.
When reviewed by the urology nurse, the patient was clearly very upset about the turn of events. Although he was reassured about the competencies of the urology team, the patient was encouraged to contact PALS if he wished to. A face-to-face appointment was also arranged with the operating surgeon who explained the events and subsequent complications. According to the surgeon, the procedure was conducted as per standard protocols, nevertheless, he apologized for the turn of events and the necessary steps for the duty of candor were taken. The patient was reassured that his fertility would not be affected and was also given the option of having a testicular prosthesis in future. The patient was satisfied with the explanation given but he was again directed towards PALS to lodge a formal complaint.
Discussion
The case revolves around a patient who underwent an orchidectomy due to post-operative complications of a hydrocele repair. The standard of care provided by the trust has been re-assessed and clinicians involved have discussed the need to ensure that adequate information is given to patients.
The patient in the case presented with a right sided scrotal swelling. He was appropriately managed by his GP who, as per the National Institute for Health and Care Excellence (NICE) guidelines, performed an ultrasound scan ruling out any sinister testicular lesions and then referred him to the urologist for a large hydrocele [6]. Since the patient had a significant and uncomfortable hydrocele, he was offered a surgical repair as per established treatment algorithms [2].
As with any surgical procedures, post-operative complications are a possibility. Effective management of complications depends on appropriate clinical examination and being aware when to order imaging to aid the diagnosis. The most common complications after hydrocelectomy include hematoma formation and post-operative infection [2],[7],[8]. The incidence of testicular injury after hydrocele repair is only 0.3% and is clinically difficult to diagnose [2]. Ultrasound scan and Doppler studies of the testis are the best image modality recommended for the diagnosis. If a testicular injury is suspected in patients with an expanding hematoma not responding to conservative management, then a surgical exploration and testicular repair are recommended within 72 hours of injury [9].
However, the patient in the case presented 7 days after the surgery. After clinically ruling out a scrotal abscess, the patient was appropriately given a course of oral antibiotics. Even if the ultrasound scan and scrotal exploration had been performed on that day, the outcome may still have been the same.
This case presentation also highlights the importance of consent for a surgical procedure. General Medical Council (GMC) UK states that “consent is a fundamental legal and ethical principle.” Patients with the mental capacity should have the right to make informed decisions about their treatment and care. The exchange of information between a clinician and the patient is essential for good decision making. At this stage, the clinician has the opportunity to find out what specificities are relevant to the patient [10].
The timing at which consent is taken is also an important factor. Department of Health recommends that for major procedures, consent should be sought well in advance to allow the patient sufficient time to process the information given and ask questions. Consent is a continuing process rather than a one-off decision.
The doctor should then confirm before the intervention that the patient is still willing to proceed with it [11].
Regarding the case presentation, the patient’s purpose for seeking treatment was mainly for a cosmetic reason. In addition, he was still a young man. He had a consultation in February 2021 and eventually had his surgery in August 2021, leaving him sufficient time to go through the information provided including a BAUS information leaflet on hydrocele repair.
It is important to note that, during the initial consultation, no mention was made of any risk of losing a testicle after a hydrocelectomy. Even, the BAUS information leaflet does not include this particular risk [8]. The risk of undergoing an orchidectomy for testicular injury after hydrocele repair is small [2]. However, in this particular patient, it can be argued that such a risk would have been of significant importance to him.
In March 2015, the United Kingdom Supreme Court (Montgomery v Lanarkshire Health Board) stated that doctors must “take reasonable care to ensure that the patient is aware of any material risks involved in any treatment, and of any reasonable alternative or variant treatments.” They went on to further define a “material risk” as one in which “a reasonable person in the patient’s position would be likely to attach significance to the risk or the doctor is or should reasonably be aware that the particular patient would be likely to attach significance to it” [3].
The only time that the patient was made aware of a risk of testicular injury was on the day of surgery. The timing at which an information is given to a patient is important.
Quoting the case of Chester (Respondent) v. Afshar (Appellant), providing the information might not have changed the patient’s decision about undergoing the procedure or the outcome but instead he would have had more time to weigh the risks and benefits and discuss matters with family members [12].
When referring to the case presentation, although all significant and material risks were given to the patient, the timing of this process may be considered less than ideal. Had the patient been aware of this risk from the start, his decision making would have been better informed. His case was discussed at the hospital’s monthly morbidity and mortality meeting. An important point raised was whether BAUS leaflet should include the risk of testicular injury in the literature even though its incidence is very low. Testicular injury and loss may be of particular significance to certain patients.
Following the incident, the urology department could have undertaken an audit for patients undergoing scrotal surgeries looking at post-operative complication rates and modifying the practice accordingly should it be required.
Conclusion
The case describes an unexpected turn of events for a patient who was undergoing a hydrocele repair for cosmetic purposes. Unfortunately, he ended up having an orchidectomy due to post-operative complications. The case highlights the importance of comprehensive and timely communication between clinicians and patients. It is a doctor’s legal and ethical duty to provide adequate information based on patients’ needs so that they make informed decisions and are satisfied with the quality of medical care.
REFERENCES
1.
Good Medical Practice. General Medical Council. 2019. [Available at: https://www.gmc-uk.org/ethical-guidance/ethical-guidance-for-doctors/good-medical-practice]

2.
Kogan BA, Erdem E. Hydrocele. BMJ Best Practice. 2020. [Available at: https://bestpractice.bmj.com/topics/en-gb/1104/pdf/1104/Hydrocele.pdf]

3.
Lord K, Lord C, Lord W, Lord R, Lord H. Montgomery (Appellant) v Lanarkshire Health Board (Respondent) (Scotland). The Supreme Court. 2015. [Available at: https://www.supremecourt.uk/cases/docs/uksc-2013-0136-judgment.pdf]

4.
Kiddoo DA, Wollin TA, Mador DR. A population based assessment of complications following outpatient hydrocelectomy and spermatocelectomy. J Urol 2004;171(2 Pt 1):746–8. [CrossRef]
[Pubmed]

5.
Kühn AL, Scortegagna E, Nowitzki KM, Kim YH. Ultrasonography of the scrotum in adults. Ultrasonography 2016;35(3):180–97. [CrossRef]
[Pubmed]

6.
Scrotal pain and swelling: Scenario: Hydrocele. NICE. 2022. [Available at: https://cks.nice.org.uk/topics/scrotal-pain-swelling/management/hydrocele/]

7.
Swartz MA, Morgan TM, Krieger JN. Complications of scrotal surgery for benign conditions. Urology 2007;69(4):616–9. [CrossRef]
[Pubmed]

8.
9.
Lucky M, Brown G, Dorkin T, et al. British Association of Urological Surgeons (BAUS) consensus document for the management of male genital emergencies - testicular trauma. BJU Int 2018;121(6):840–4. [CrossRef]
[Pubmed]

10.
Guidance on professional standards and ethics for doctors: Decision making and consent. General Medical Council. 2020. [Available at: https://www.gmc-uk.org/ethical-guidance/ethical-guidance-for-doctors/decision-making-and-consent]

11.
Department of Health. Reference guide to consent for examination or treatment. Second edition. 2009. [Available at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/138296/dh_103653__1_.pdf]

12.
Judgments - Chester (Respondent) v. Afshar (Appellant). House of Lords, Publication on the internet, Judgements. 2004. [Available at: https://publications.parliament.uk/pa/ld200304/ldjudgmt/jd041014/cheste-1.htm]

SUPPORTING INFORMATION
Acknowledgments
Mr Ben Dawam Urology Consultant
Author ContributionsDivya Bheenick - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthor declares no conflict of interest.
Copyright© 2022 Divya Bheenick. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.