|
Case Report
An uncommon infection after transurethral resection for bladder tumor: Emphysematous cystitis
1 Department of Urology, Faculty of Medicine, Adiyaman University, Adiyaman, Turkey
Address correspondence to:
Ferhat Çoban
Department of Urology, Faculty of Medicine, Adiyaman University, Adiyaman 02000,
Turkey
Message to Corresponding Author
Article ID: 100056Z15FC2025
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Çoban F. An uncommon infection after transurethral resection for bladder tumor: Emphysematous cystitis. J Case Rep Images Urol 2025;10(2):10–13.ABSTRACT
Introduction: Emphysematous cystitis (EC) is a rare but potentially life-threatening form of complicated urinary tract infection, typically associated with diabetes mellitus and urological instrumentation. Computed tomography is considered the most sensitive diagnostic tool.
Case Report: We present a 51-year-old male with a history of diabetes mellitus who developed EC three weeks after undergoing transurethral resection (TUR) for a large bladder tumor. The patient was admitted with severe dysuria and suprapubic pain. Laboratory findings were leukocytosis, hyperglycemia, elevated C-reactive protein, and impaired renal function. Computed tomography (CT) revealed diffuse bladder wall thickening and intramural air densities localized at the previous TUR site. Broad-spectrum intravenous antibiotics, bladder drainage with an indwelling catheter, and daily bladder irrigation were performed. No pathogens grew in urine and blood cultures. After 14 days, clinical and radiological findings completely resolved.
Conclusion: Emphysematous cystitis is an uncommon, but serious infection that can develop after urological interventions such as TUR. Early diagnosis with CT, prompt antibiotic therapy, and effective bladder drainage are essential for favorable outcomes. Clinicians should be aware of this possibility in patients with diabetes undergoing extensive bladder tumor resections.
Keywords: Emphysematous cystitis, Pneumaturia, Transurethral resection, Urinary tract infections
Introduction
Emphysematous cystitis is an uncommon yet potentially life-threatening infection marked by the presence of gas within the bladder wall and lumen, resulting from gas-producing microorganisms such as Escherichia coli, Klebsiella pneumoniae, Enterobacter aerogenes, Proteus mirabilis, Streptococcus species, and Clostridium perfringens [1],[2]. Diabetes mellitus (DM), found in roughly 60–65% of cases, is regarded as the most critical risk factor. The condition is reported to be twice as common in females compared to males. Other risk factors include advanced age, neurogenic bladder, recurrent UTIs, urinary stasis due to bladder outlet obstruction, and recent urological instrumentation [3].
Case Report
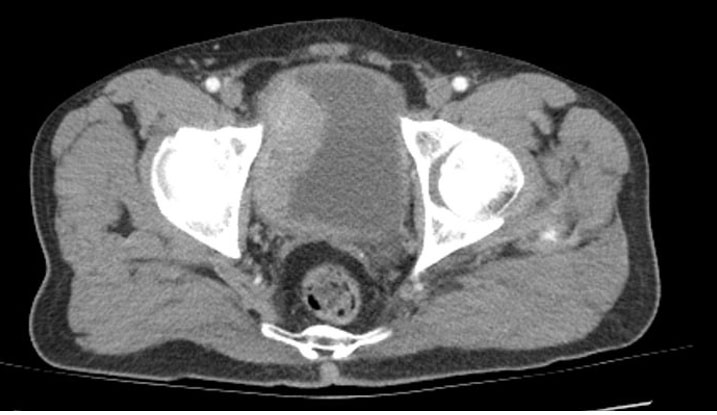
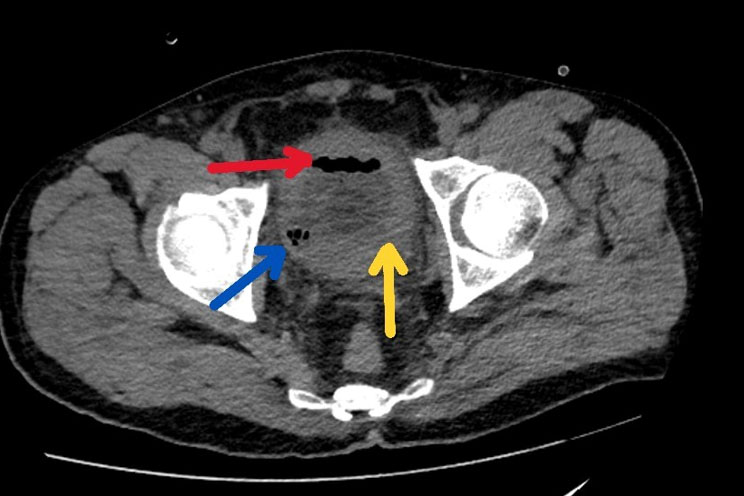
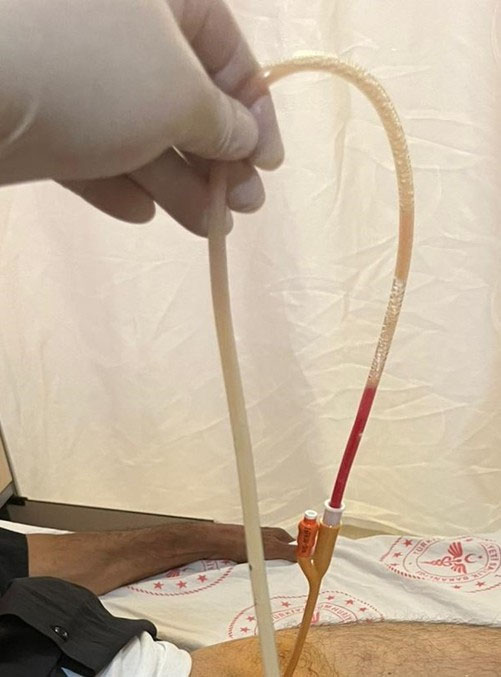
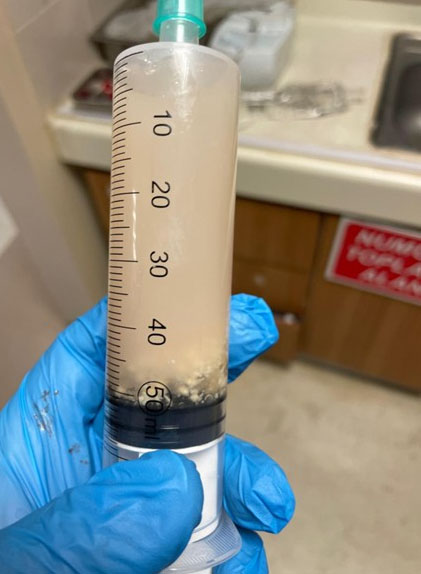
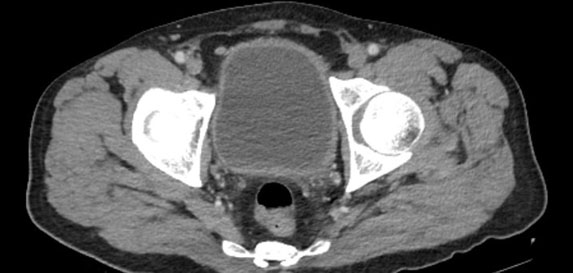
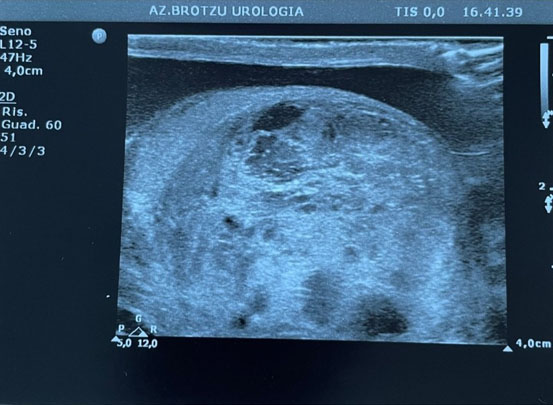
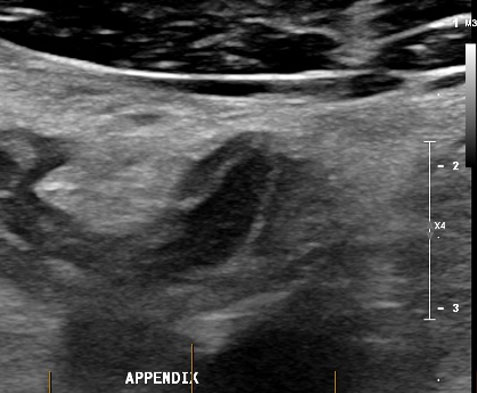
A 51-year-old male patient visited the urology outpatient clinic due to severe dysuria. It was discovered that he had previously under gone non-contrast CT because of macroscopic hematuria, which identified a tumor-like mass approximately 6 cm in diameter on the right lateral wall of the bladder (Figure 1). Consequently, the patient had a TUR of the tumor three weeks earlier and was discharged without any complications. His medical history included type 2 DM, diagnosed a decade ago. During the physical examination, the patient showed diffuse tenderness and pain in the suprapubic area. The patient had no fever at the time of admission. Laboratory results indicated a leukocyte count of 13,230/mm³ (reference: 4,300–10,300/mm³), a glucose level of 175 mg/dL (reference: 70–110 mg/dL), C-reactive protein of 14.8 mg/dL (reference: 0–0.5 mg/dL), HbA1c of 8.6% (reference: 4%–6%), and a creatinine level of 2.14 mg/dL (reference: 0.5–1.3 mg/dL). Urine analysis showed +3 erythrocytes and +3 leukocytes upon microscopic examination. His preoperative urine culture was sterile. The biochemical urine analysis revealed +2 protein and +3 glucose. No abnormalities were found in the urinary system ultrasonography (US). Given the initial diagnosis of a complicated UTI, a non-contrast abdominopelvic CT was conducted. On CT, diffuse thickening of all bladder walls and the presence of intramural air densities were noted within the bladder lumen, particularly in the area of the previous TUR on the right lateral bladder wall (Figure 2). The patient was admitted to the urology unit. Urine and blood cultures were taken. Intravenous broad-spectrum antibiotic treatment was initiated with meropenem at 1000 mg twice daily and moxifloxacin at 400 mg once daily. An 18 Fr urethral catheter was inserted for bladder drainage. Following catheterization, pneumaturia was observed (Figure 3). Bladder irrigation was conducted using normal saline. During the irrigation process, thick, foul-smelling infected urine containing solid particles was observed draining from the bladder (Figure 4). Irrigation continued until the urine was clear. During the follow-up in the ward, intermittent blockage of the catheter was noted. Therefore, daily bladder irrigation was continued. No microbial growth was detected in either urine or blood cultures. After 14 days of intravenous antibiotic treatment and continuous bladder drainage, the patient’s symptoms completely resolved, and laboratory values normalized. Follow-up imaging showed complete resolution of the previously observed diffuse bladder wall thickening and intramural air densities, and the patient was discharged in good condition (Figure 5).
Discussion
The treatment of EC and emphysematous pyelonephritis (EPN) is of utmost clinical importance due to their potential for rapid progression and high mortality. While EC is generally managed successfully with conservative measures such as broad-spectrum antibiotics, strict glycemic control, bladder drainage, and, when necessary, bladder irrigation, EPN often requires a more aggressive approach. In addition to antimicrobial therapy, percutaneous drainage or even nephrectomy may be required in severe cases to achieve infection control and prevent septic complications. Prompt recognition and appropriate treatment are critical, as delays are strongly associated with adverse outcomes. The literature emphasizes that although EC carries a relatively favorable prognosis with early management, EPN remains a life-threatening condition, highlighting the need for vigilant diagnostic assessment and individualized treatment strategies [1],[2],[3].
Emphysematous cystitis is a rare and intricate UTI characterized by the presence of gas in the bladder lumen and bladder wall [4]. It may present either asymptomatically or with pronounced septic signs. The primary symptoms of EC include abdominal pain, suprapubic discomfort, urinary retention, dysuria, increased urination frequency, urgency, hematuria, and pneumaturia. A study by Moti Grubber et al. found that at least one of these primary symptoms was observed in 53.3% of the patients. Additionally, the same study reported a 70% incidence of pneumaturia following catheterization [5]. In the case we reviewed, the only symptom exhibited was dysuria. Pneumaturia was also observed after the catheter was inserted.
Among the most common predisposing factors for complicated UTIs are DM, neurogenic bladder, urological instrumentation, and bladder outlet obstructions that result in urinary stasis [6]. A literature review conducted by Anil A. Thomas et al., which included 135 cases, indicated that 64% of the patients were female, and 67% had received a diagnosis of DM [1]. The case we presented involved a male patient with a history of DM, as well as recent urinary intervention and instrumentation. In our literature review, we did not identify any previously documented instances of EC occurring following TUR.
While Escherichia coli is recognized as the most prevalent pathogen, Klebsiella pneumoniae holds the second position. Additional causative agents consist of Enterococcus, Candida, and Clostridium perfringens [5]. In our instance, no growth was detected in the culture studies.
Conventional radiography and abdominopelvic CT are prominent in the diagnostic process. In the study conducted by Anil A. Thomas et al., diagnosis was made using plain abdominal radiography in 84% of the patients, CT in 40%, and ultrasound (US) in 7% [1]. Computed tomography is considered the most sensitive and specific diagnostic tool, particularly due to its ability to reveal potential conditions such as vesicocolic fistula, vesicovaginal fistula, and intra-abdominal abscesses [1],[5]. In our case, the initial ultrasound was insufficient for diagnosis. The definitive diagnosis was established via abdominopelvic CT.
Treatment success in EC depends on early diagnosis, correction of predisposing factors, prompt and empiric administration of broad-spectrum antibiotics considering potential pathogens, adequate bladder drainage, and surgical removal of affected tissue when necessary. Approximately 90% of patients can be treated with medical therapy alone, while 10% require a combination of medical and surgical treatment. The mortality rate is around 7% [1]. In the present case, treatment was achieved through effective bladder drainage (including bladder irrigation via catheter when necessary) and antibiotic therapy.
Conclusion
Emphysematous cystitis is a serious, potentially life-threatening form of complicated UTI. Computed tomography is considered the first-line imaging modality for diagnosis, as it can also reveal possible associated complications. While DM is the most common underlying cause, the condition can also develop following urological instrumentation. To date, EC occurring after TUR has not been reported in the literature. In patients with extensive bladder tumors, the possibility of developing EC following a wide-based resection should be kept in mind.
REFERENCES
1.
Thomas AA, Lane BR, Thomas AZ, Remer EM, Campbell SC, Shoskes DA. Emphysematous cystitis: A review of 135 cases. BJU Int 2007;100(1):17–20. [CrossRef]
[Pubmed]

2.
Quint HJ, Drach GW, Rappaport WD, Hoffmann CJ. Emphysematous cystitis: A review of the spectrum of disease. J Urol 1992;147(1):134–7. [CrossRef]
[Pubmed]

3.
Schicho A, Stroszczynski C, Wiggermann P. Emphysematous cystitis: Mortality, risk factors, and pathogens of a rare disease. Clin Pract 2017;7(2):930. [CrossRef]
[Pubmed]

4.
Amano M, Shimizu T. Emphysematous cystitis: A review of the literature. Intern Med 2014;53(2):79–82. [CrossRef]
[Pubmed]

5.
Grupper M, Kravtsov A, Potasman I. Emphysematous cystitis: Illustrative case report and review of the literature. Medicine (Baltimore) 2007;86(1):47–53. [CrossRef]
[Pubmed]

6.
Wagenlehner FME, Bjerklund Johansen TE, Cai T, Koves B, Kranz J, Pilatz A, Tandogdu Z. Epidemiology, definition and treatment of complicated urinary tract infections. Nat Rev Urol 2020;17(10):586–600. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Acknowledgments
No generative artificial intelligence tools were used in the preparation of this study.
Author ContributionsFerhat Çoban - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthor declares no conflict of interest.
Copyright© 2025 Ferhat Çoban. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.