|
Clinical Image
Atypical acute obstruction of the urinary tract
1 MD, Nephrology Unit, University Hospital of Reunion Island Saint Denis, La Réunion, France
2 MD, Radiology Department, University Hospital of Reunion Island Saint Pierre, La Réunion, France
3 MD, Critical Care Unit, University Hospital of Reunion Island Saint Pierre, La Réunion, France
Address correspondence to:
Marie Julien
Félix-Guyon University Hospital of La Réunion, Allée des topazes, Saint Denis, Réunion Island,
France
Message to Corresponding Author
Article ID: 100047Z15MJ2024
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Julien M, El Ramadan S, Rager G. Atypical acute obstruction of the urinary tract. J Case Rep Images Urol 2024;9(2):9–11.ABSTRACT
No Abstract
Keywords: Acute kidney injury, Curvilinear reconstruction, Ureteral obstruction, Urinary catheter
Case Report
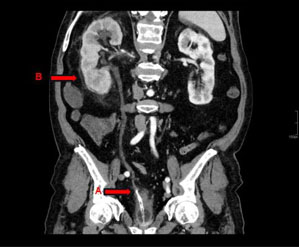
A 71-year-old man with a history of untreated prostate adenocarcinoma and an indwelling urinary catheter (UC) for chronic urinary retention was admitted to the intensive care unit for septic shock. He presented a significant biological inflammatory syndrome, hyperlactatemia of 3.4 mmol/L and stage 1 acute kidney injury. During the exploration, the patient underwent an abdominal computed tomography (CT) scan. The scan revealed dilatation of the right urinary tract due to obstruction of the right ureteral orifice by the end of the Foley tube as seen on the curvilinear reconstruction (Figure 1).
Fatty infiltration due to obstruction was observed around the right kidney, as well as mild late contrast enhancement in the parenchyma. This indwelling UC was removed and replaced upon admission to our department. The patient did well under empiric antibiotic therapy, resulting in the normalization of renal function. Subsequently, he was referred to the urological surgery unit to plan a prostatectomy.
Discussion
Most ureteral lesions are caused by medical procedures, such as those performed by urologists, gynecologists, or general surgical procedures, or by external trauma [1],[2]. Ureteral obstruction due to UC is a rare clinical event with fewer than 30 cases reported worldwide [3].
Female gender, neurogenic bladder, sensory disturbances, and urethral catheterization with an empty bladder appear to increase the likehood of UC ureteral malposition [4],[5].
Ultrasound, CT, and cystoscopy are diagnostic tools for suspected catheter misplacement [6] . The Foley catheter appears as a hypodense spherical structure filled with water attenuation on CT. Hydroureteronephrosis may also be observed, especially when Foley catheter is placed at the ureteral orifice. Contrast-enhanced CT urography or magnetic resonance imaging may be useful in the diagnosis of ureteral rupture with contrast leakage into the abdomen and pelvis [7].
If the ureter is not injured, patients can be managed conservatively by changing or removing the catheter and treating any urinary tract infection.
In cases of ureteral dilaceration or rupture may require endoscopic surgery, percutaneous nephrostomy, or laparotomy for reconstruction [3],[8].
Conclusion
Urinary catheter ureteral malposition is a very rare clinical entity that can result in severe complications. Diagnosis can be quickly made through imaging to visualize a misplaced catheter or secondary hydroureteronephrosis. Conservative management is possible if the ureter remains intact.
REFERENCES
1.
Elliott SP, McAninch JW. Ureteral injuries from external violence: The 25-year experience at San Francisco General Hospital. J Urol 2003;170(4 Pt 1):1213–6. [CrossRef]
[Pubmed]

2.
Selzman AA, Spirnak JP. Iatrogenic ureteral injuries: A 20-year experience in treating 165 injuries. J Urol 1996;155(3):878–81. [CrossRef]
[Pubmed]

3.
Qin PF, Liu WZ, Yang BB, et al. Removal of a Foley catheter misplaced into the ureter by percutaneous puncture: A rare case report. BMC Urol 2022;22(1):99. [CrossRef]
[Pubmed]

4.
Ishikawa T, Araki M, Hirata T, et al. A rare complication: Misdirection of an indwelling urethral catheter into the ureter. Acta Med Okayama 2014;68(1):47–51. [CrossRef]
[Pubmed]

5.
Lowthian P. Aberrant Foley catheter placement into the proximal right ureter. BJU Int 2002;90(4):475–6. [CrossRef]
[Pubmed]

6.
Danaie M, Nezameslami A, Mishan M, Mehdikhani B, Mansouri Z. Misplaced urinary catheter in the ectopic ureter in a female with previously undiagnosed duplex ureter: A rare case. Cureus 2022;14(11):e31139. [CrossRef]
[Pubmed]

7.
Baker KS, Dane B, Edelstein Y, Malhotra A, Gould E. Ureteral rupture from aberrant Foley catheter placement: A case report. J Radiol Case Rep 2013;7(1):33–40. [CrossRef]
[Pubmed]

8.
Bryk DJ, Zhao LC. Guideline of guidelines: A review of urological trauma guidelines. BJU Int 2016;117(2):226–34. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Marie Julien - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Sami El Ramadan - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Gwendoline Rager - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2024 Marie Julien et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.