|
Case Report
Pulmonary alveolar microlithiasis with calcifications in the seminal vesicles and prostate causing infertility: A case report
1 Pneumo-phthisiology Department, Moulay Youssef Hospital, Faculty of Medicine and Pharmacy of Rabat, Morocco
Address correspondence to:
Nezha Reguig
Pneumo-phthisiology Department, Moulay Youssef Hospital, Faculty of Medicine and Pharmacy of Rabat,
Morocco
Message to Corresponding Author
Article ID: 100045Z15NR2024
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Reguig N, Messaoudi MA, Omari W, Aharmim M, Soualhi M, Zahraoui R. Pulmonary alveolar microlithiasis with calcifications in the seminal vesicles and prostate causing infertility: A case report. J Case Rep Images Urol 2024;9(2):1–4.ABSTRACT
Introduction: Pulmonary alveolar microlithiasis (PAM) is a rare hereditary disease caused by the mutation of the SLC34A2 gene, characterized by the deposition of calcium phosphate microliths throughout the alveolar spaces. Calcifications have also been reported in other organs such as the genitalia of male patients and can be associated with infertility cases. Our case report is the first Moroccan case reported in the literature of a male with PAM and infertility.
Case Report: We present a case of a 47-year-old male patient (Moroccan, North African) presented with complaints of persistent grade I dyspnea for the last six years. He also claimed primary infertility of 20 years since marriage, PAM was diagnosed based on the typical appearance of the chest and pelvic high resolution computed tomography (HRCT). The infertility was due to distal obstruction of the seminal tract by small calcifications similar to pulmonary microliths. Low dose inhaled corticosteroids/long-acting beta2-agonists (ICS-LABA) was started as a treatment of symptoms with good control of symptoms.
Conclusion: Pulmonary alveolar microlithiasis is a rare autosomal recessive disorder not easily described because of its rarity worldwide, its clinical course, and its evolution. Its association with infertility may be more common than is currently known, suggests the need to make a particularly close examination of the chest X-ray in some cases of male infertility.
Keywords: Hereditary disease, Infertility, Oligoasthenospermia, Prostate, Pulmonary alveolar microlithiasis, Seminal vesicles
Introduction
Pulmonary alveolar microlithiasis (PAM) is a rare hereditary disease caused by the mutation of the SLC34A2 gene. It is characterized by the diffuse presence in the pulmonary alveoli of microliths made of calcium phosphate. It presents a wide spectrum from patients being asymptomatic for many decades to patients suffering from progressive respiratory failure and death [1]. The disease is often discovered incidentally in asymptomatic subjects in middle age.
Calcifications have also been reported in other organs such as the genitalia of male patients with PAM and can be associated with infertility cases.
We report a case of a patient with severe oligoasthenospermia due to distal obstruction of the seminal tract associated with PAM.
Case Report
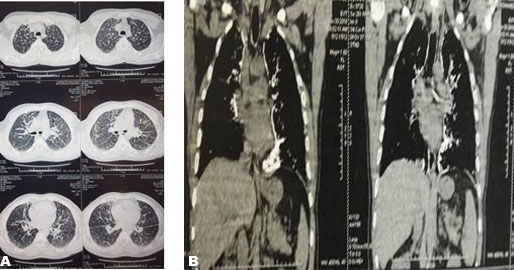
A 47-year-old male patient from a non-consanguineous family, who has never smoked, presented with complaints of persistent grade I dyspnea for the last six years, the physical examination was normal but later revealed wheezing groans, the chest X-ray revealed a bilaterally diffuse interstitial infiltrate (Figure 1), and the HRCT of the lungs showed diffuse, hyperdense micronodules throughout the whole lungs accompanied with bilateral calcific pleural thickening (Figure 2A and Figure 2B). Routine blood tests including serum phosphate and calcium were normal. The patient underwent bronchoscopy with broncho-alveolar lavage but did not demonstrate the characteristic microliths. Tuberculosis was ruled out due to the absence of acid-fast bacilli detection (Ziehl–Neelsen stain) in the lavage. Other differential diagnoses like asbestosis and hyperparathyroidism were ruled out.
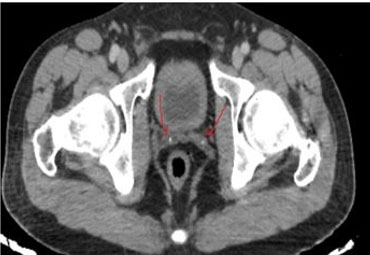
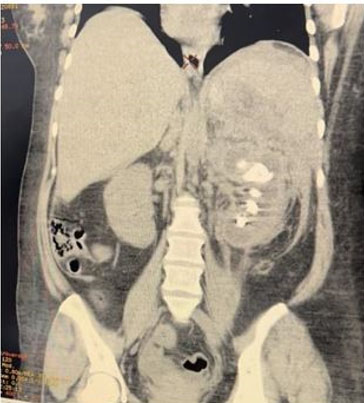
Otherwise, the patient claims primary infertility of 20 years since marriage, he underwent a spermiogram that revealed oligoasthenospermia. Pelvic computed tomography (CT) scans showed calcifications in the prostate (Figure 3) and seminal vesicles (Figure 4), pelvis magnetic resonance imaging (MRI) scan confirmed the CT scan findings.
Based on the typical appearance of chest and pelvic HRCT, the patient was diagnosed with PMA.
Pulmonary function tests were normal at first but later revealed an obstructive ventilatory defect.
So far, the patient is stable with effective control of symptoms (dyspnea and wheeze) on low-dose ICS-LABA therapy, with no clinical worsening observed. Gene testing was not performed on this patient due to economic constraints.
Discussion
Pulmonary alveolar microlithiasis is a rare disease characterized by the deposition of calcium phosphate microliths throughout the alveolar spaces. More than 1000 cases have been reported worldwide, the majority of cases have been from Asia (576 cases; 56.3%) followed by Europe; in Africa, 38 cases were reported with 14 cases in Morocco [2].
Pulmonary alveolar microlithiasis is a typical example of clinical and radiological dissociation, with significant heterogeneity in disease onset, symptoms, and natural course. Patients maybe asymptomatic for many years, the disease most often becomes symptomatic in the fourth to fifth decade.
The main clinical symptoms are non-productive cough, dyspnea, chest pain but pneumothorax remain rare [3]. Respiratory failure, pulmonary hypertension, and fibrosis may develop overtime [4].
Computed tomography of the chest stands out as the main radiological method for diagnosing PAM. Findings on HRCT can be categorized into four stages based on the degree of radiologic severity [5]. The initial phase, described as pre-calcific, lacks the typical appearance due to the small number and smaller size of the calcifications. The second phase exhibits the characteristic “sandstorm” appearance with diffusely scattered calcific micronodules. The microliths tend to distribute throughout the lungs, with a higher concentration typically observed in the medial and inferior regions. The third phase demonstrates an increased number and volume of opacifications, as well as interstitial thickening [4]. Ground-glass opacity with thickening interlobular septa can sometimes produce the so-called “crazy-paving” sign [6]. The fourth stage is characterized by a notable advance in the number and size of calcific deposits, resulting in intense calcification of the interstitium and pleural serosa, which gives the overall appearance of “white lungs” [7].
Pulmonary alveolar microlithiasis is considered a genetic disease due to the inactivating mutations within the SLC34A2 gene. It is primarily expressed in alveolar type II cells, but it is also expressed in other epithelial tissues, including mammary glands, the small intestine, kidneys, pancreas, ovaries, liver, testes, placenta, and prostate [8].
In the majority of cases documented in the literature, PAM is confined to the lungs, but many case reports have described the potential association of calcifications in the genitalia of male patients with PAM: Coetzee [9] reported a case of PAM with extrapulmonary microliths in the testicles and in the sympathetic ganglia. Sandhyamani et al. [10], Arslan et al. [11], and Castellana et al. [12] described respectively cases of PAM with the microliths present in the seminal vesicles, Kanat et al. [13] reported a 37-year-old male patient with PAM and microliths in the head of the epididymides and in the periurethral tissue.
Testicular microlithiasis has a prevalence of 0.6–0.9% in the general male population, can be associated with up to 1% of all idiopathic infertility cases, and has been linked to testicular malignancies. Testicular microlithiasis can lead to bilateral testicular atrophy and obstructive azoospermia [14].
Our case report is the first Moroccan case reported in the literature of a male with PAM and infertility due to oligoasthenospermia, caused by the microliths present in the seminal vesicles and the prostate. In Morocco, PAM is misdiagnosed as tuberculosis or silicosis, and also the difficulty to carry out genetic tests because of their price which is quite expensive.
Our patient was put under ICS-LABA association seeing the presence of an obstructive ventilatory defect with good control of symptoms (wheezing and dyspnea), he consults every three months with clinical and functional control. So far, he is stable with no clinical worsening. Annual scanning control is planned to monitor the patient’s condition.
Conclusion
Pulmonary alveolar microlithiasis is a rare autosomal recessive disorder not easily described because of its rarity worldwide, its clinical course, and its evolution. Its association with infertility may be more common than is currently known, suggests the need to make a particularly close examination of the chest X-ray in some cases of male infertility.
Pulmonary alveolar microlithiasis should be included in the list of chronic pulmonary diseases associated with sterility.
REFERENCES
1.
Bendstrup E, Jönsson ÅLM. Pulmonary alveolar microlithiasis: No longer in the stone age. ERJ Open Res 2020;6(3):00289–2020. [CrossRef]
[Pubmed]

2.
Castellana G, Castellana G, Gentile M, Castellana R, Resta O. Pulmonary alveolar microlithiasis: Review of the 1022 cases reported worldwide. Eur Respir Rev 2015;24(138):607–20. [CrossRef]
[Pubmed]

3.
Enemark A, Jönsson ÅLM, Kronborg-White S, Bendstrup E. Pulmonary alveolar microlithiasis – A review. Yale J Biol Med 2021;94(4):637–44.
[Pubmed]

4.
Mascie-Taylor BH, Wardman AG, Madden CA, Page RL. A case of alveolar microlithiasis: Observation over 22 years and recovery of material by lavage. Thorax 1985;40(12):952–3. [CrossRef]
[Pubmed]

5.
Castellana G, Castellana R, Fanelli C, Lamorgese V, Florio C. Pulmonary alveolar microlithiasis: Clinical and radiological course of three cases according to conventional radiology and HRCT. A hypothesis for radiological classification. Radiol Med 2003;106(3):160–8.
[Pubmed]

6.
Gasparetto EL, Tazoniero P, Escuissato DL, Marchiori E, Frare E Silva RL, Sakamoto D. Pulmonary alveolar microlithiasis presenting with crazy-paving pattern on high resolution CT. Br J Radiol 2004;77(923):974–6. [CrossRef]
[Pubmed]

7.
Zhang XD, Gao JM, Luo JM, Zhao Y. Pulmonary alveolar microlithiasis: A case report and review of the literature. Exp Ther Med 2018;15:831–7 [CrossRef]

8.
Nishimura M, Naito S. Tissue-specific mRNA expression profiles of human solute carrier transporter superfamilies. Drug Metab Pharmacokinet 2008;23(1):22–44. [CrossRef]
[Pubmed]

9.
Coetzee T. Pulmonary alveolar microlithiasis with involvement of the sympathetic nervous system and gonads. Thorax 1970;25(5):637–42. [CrossRef]
[Pubmed]

10.
Sandhyamani S, Verma K, Sharma SK, Pande JN. Pulmonary alveolar microlithiasis. Indian J Chest Dis Allied Sci 1982;24(1):33–5.
[Pubmed]

11.
Arslan A, Yalin T, Akan H, Belet U. Pulmonary alveolar microlithiasis associated with calcifications in the seminal vesicles. J Belge Radiol 1996;79(3):118–9.
[Pubmed]

12.
13.
Kanat F, Teke T, Imecik O. Pulmonary alveolar microlithiasis with epididymal and periurethral calcifications causing obstructive azospermia. Int J Tuberc Lung Dis 2004;8(10):1275.
[Pubmed]

14.
Kosciuk P, Meyer C, Wikenheiser-Brokamp KA, McCormack FX. Pulmonary alveolar microlithiasis. Eur Respir Rev 2020;29(158):200024. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Nezha Reguig - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Mohamed Anouar Messaoudi - Acquisition of data, Analysis of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Wafae Omari - Acquisition of data, Analysis of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Mohammed Aharmim - Conception of the work, Design of the work, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Mouna Soualhi - Conception of the work, Design of the work, Acquisition of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Rachida Zahraoui - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2024 Nezha Reguig et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.