|
Case Report
Transient flank bulge after percutaneous nephrolithotomy
1 Deputy Director for Medical Affairs (Urology), Department of Urology, Saint-Petersburg State University Hospital, Saint-Petersburg, Russia
2 Urologist, Department of Urology, Saint-Petersburg State University Hospital, Saint-Petersburg, Russia
3 Urologist, Department of Urology, Saint-Petersburg State University Hospital, Saint- Petersburg, Russia
4 Head of Department of Urology, Department of Urology, Saint-Petersburg State University Hospital, Saint-Petersburg, Russia
Address correspondence to:
Aram Aloyan
Komendantskiy pr. 12-1-113, 197372 Saint-Petersburg,
Russia
Message to Corresponding Author
Article ID: 100032Z15NG2023
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Gadzhiev N, Aloyan A, Petrov A, Gorgotsky I, Shkarupa A. Transient flank bulge after percutaneous nephrolithotomy. J Case Rep Images Urol 2023;8(1):17–19.ABSTRACT
Introduction: Percutaneous nephrolithotomy (PCNL) is considered as the “gold standard” treatment for large (>2 cm) and complex kidney stones. We present a case of transient tone loss of the anterolateral abdominal wall, which is a rare complication after PCNL.
Case Report: A 50-year-old male with a complete staghorn stone of the right kidney underwent standard PCNL in prone position at the 11th intercostal space. On the 6th post-operative day the patient complained on painless bulge in the right flank. Computed tomography (CT) scan in supine position revealed no signs of herniation, retroperitoneal hematoma, or residual fragments. Flank bulge was attributed to the muscle tone loss either because of the 11th intercostal nerve injury by the needle or nerve compression by the Amplatz sheath. Within next six months flank bulge has completely resolved.
Conclusion: Flank bulge after PCNL although rare but possible and transient condition. Nerve injury seems to be the most likely cause.
Keywords: Complications, Flank bulge, Percutaneous nephrolithotomy, Urolithiasis
Introduction
Percutaneous nephrolithotomy (PCNL) has replaced open surgery and is considered as the “gold standard” treatment for large (>2 cm) and complex kidney stones [1]. A common complication of open surgery is the loss of tone of the anterolateral abdominal wall muscles due to nerve injury which looks like a flank bulge [2],[3],[4],[5]. Although PCNL is perceived as minimally invasive option nerve injury is still a possible complication [6]. We present a case of transient tone loss of the anterolateral abdominal wall after PCNL, which has resolved spontaneously within six months.
Case Report
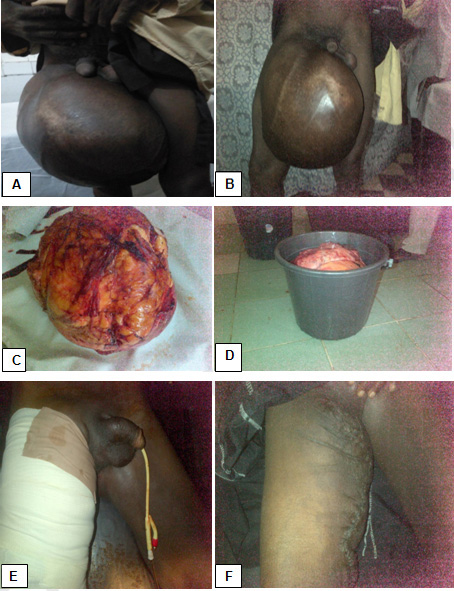
A 50-year-old male presented with right flank pain and hematuria. Computed tomography revealed a complete staghorn stone of the right kidney. The patient underwent single tract standard PCNL in prone position at the 11th intercostal (IC) space 3 cm medial from posterior axillary line with 30° puncture angle and was sequentially dilated up to 30 Ch. Total operative time was 85 minutes and completed with nephrostomy tube 12 Fr. Early postoperative period was uneventful. The patient was discharged on the 3rd postoperative day (POD) with nephrostomy tube. However, on the 6th POD patient was readmitted with complains on painless bulge in the right flank. No history of fever or pain was noted. Computed tomography scan in supine position revealed no signs of herniation, retroperitoneal hematoma, or residual fragments. Flank bulge was attributed to the muscle tone loss. The patient was discharged on the next day without any specific recommendations. Within next six months the bulge has completely resolved (Figure 1).
Discussion
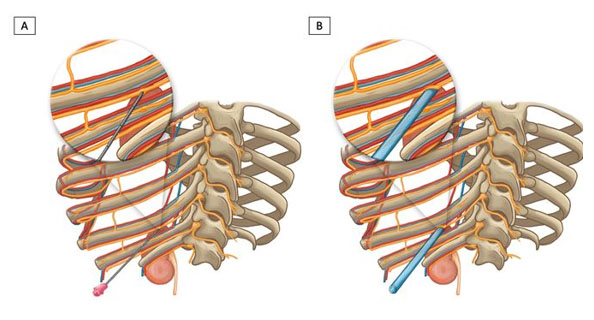
In the era of endoscopy open surgery for kidney stones has become rather obsolete [7],[8]. Nerve injury during lumbotomy can lead to the muscle tone loss of the abdominal wall [2],[3]. Rarely nerves can be injured during PCNL either by direct needle hit during puncture or nerve compression between the Amplatz sheath and the rib (Figure 2). Intercostal (IC) neurovascular bundle courses mainly along the inferior margin of each rib and passes inferior from the 11th rib as it progresses lateral. Despite this, it is further from the 12th rib than from 11th one. Thus, puncture in the lower half of the IC space is potentially safer regarding IC nerve injury [6]. Up to now only three cases of flank muscle tone loss after PCNL are described in the literature [9],[10]. Two of them were performed in prone-flexed position through supracostal (12th rib) access and 12th intercostal space, respectively, to upper calyces without nephrostomy drainage [9]. Third case was performed through subcostal access to lower calyx in prone position with nephrostomy drainage after the surgery [10]. Two out of three described flank bulges have resolved on their own with time. Our case proves the transient character of the flank bulge caused by the nerve damage during PCNL. As most flank bulges are reversible, PCNL is more likely to cause a nerve compression than a nerve transection.
Conclusion
Flank bulge after PCNL although rare but possible and transient condition. Nerve injury seems to be the most likely cause.
REFERENCES
1.
Türk C, Petøík A, Sarica K, et al. EAU guidelines on interventional treatment for urolithiasis. Eur Urol 2016;69(3):475–82. [CrossRef]
[Pubmed]

2.
Gardner GP, Josephs LG, Rosca M, Rich J, Woodson J, Menzoian JO. The retroperitoneal incision. An evaluation of postoperative flank ‘bulge’. Arch Surg 1994;129(7):753–6. [CrossRef]
[Pubmed]

3.
Chatterjee S, Nam R, Fleshner N, Klotz L. Permanent flank bulge is a consequence of flank incision for radical nephrectomy in one half of patients. Urol Oncol 2004;22(1):36–9. [CrossRef]
[Pubmed]

4.
Hoffman RS, Smink DS, Noone RB, Noone RB Jr, Smink RD Jr. Surgical repair of the abdominal bulge: Correction of a complication of the flank incision for retroperitoneal surgery. J Am Coll Surg 2004;199(5):830–5. [CrossRef]
[Pubmed]

5.
Zhou DJ, Carlson MA. Incidence, etiology, management, and outcomes of flank hernia: Review of published data. Hernia 2018;22(2):353–61. [CrossRef]
[Pubmed]

6.
McAllister M, Lim K, Torrey R, Chenoweth J, Barker B, Baldwin DD. Intercostal vessels and nerves are at risk for injury during supracostal percutaneous nephrostolithotomy. J Urol 2011;185(1):329–34. [CrossRef]
[Pubmed]

7.
Alivizatos G, Skolarikos A. Is there still a role for open surgery in the management of renal stones? Curr Opin Urol 2006;16(2):106–11. [CrossRef]
[Pubmed]

8.
El-Husseiny T, Buchholz N. The role of open stone surgery. Arab J Urol 2012;10(3):284–8. [CrossRef]
[Pubmed]

9.
Lantz AG, Pace KT, Honey RJ. Flank bulge following supracostal percutaneous nephrolithotomy: A report of 2 cases. Can Urol Assoc J 2013;7(7–8):E547–9. [CrossRef]
[Pubmed]

10.
Chakraborty JN, Deb A. Flank bulge following subcostal percutaneous nephrolithotomy. Res Rep Urol 2018;10:195–7. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Acknowledgments
This research has received no external funding.
Author ContributionsNariman Gadzhiev - Conception of the work, Design of the work, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Aram Aloyan - Acquisition of data, Analysis of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Alexandr Petrov - Acquisition of data, Analysis of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ivan Gorgotsky - Acquisition of data, Analysis of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Andrei Shkarupa - Acquisition of data, Analysis of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2023 Nariman Gadzhiev et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.