|
Case Report
A cavernous hemangioma in an adrenal gland
1 Department of Urology, International University of Health and Welfare (IUHW), Hospital, Tochigi, Japan
2 Department of Pathology, International University of Health and Welfare (IUHW), Hospital, Tochigi, Japan
3 Senior Professor, Department of Renal and Urological Surgery, International University of Health and Welfare (IUHW), Chiba, Japan
Address correspondence to:
Ei-Ichiro Takaoka
Department of Urology, International University of Health and Welfare (IUHW) Hospital, Iguchi 537-3, Nasushiobara-shi, Tochigi 329-2763,
Japan
Message to Corresponding Author
Article ID: 100019Z15TA2021
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Ando T, Takaoka E-I, Inai H, Okada S, Uchida K, Miyazaki J. A cavernous hemangioma in an adrenal gland. J Case Rep Images Urol 2021;6:100019Z15TA2021.ABSTRACT
Introduction: Cavernous hemangioma is a relatively rare, non-functional, benign adrenal tumor. It is difficult to distinguish from pheochromocytoma or adrenal cancer by preoperative imaging studies.
Case Report: A 66-year-old Japanese man was hospitalized for treatment of a left adrenal tumor. The 15-mm-long tumor was identified accidentally in July 2015 and had been grown to 28 mm by July 2020, confirmed by computed tomography. The laboratory examination including hormonal variables revealed no abnormality. Since the tumor had been growing and malignancy was possible, a radical left adrenalectomy was performed. The pathological diagnosis was cavernous hemangioma of the left adrenal gland.
Conclusion: Cavernous hemangioma should be considered as one of the differential diagnoses of non-functional adrenal accidental tumors with varying sizes.
Keywords: Adrenal incidentaloma, Cavernous hemangioma, Non-functional tumor
Introduction
Cavernous hemangioma of the adrenal gland is an uncommon, benign vascular tumor. About 200 cases have been reported in the literature since Virchow first described it in 1867 [1]. Our case was found as adrenal incidentaloma in 2015 as mentioned in the following “CASE REPORT” section. Adrenal incidentaloma is an adrenal lesion larger than 1 cm in diameter discovered incidentally on imaging not suspected adrenal disease. Differential diagnoses of common causes of adrenal incidentalomas are tumor, hyperplasia, metastases, infection, hemorrhages, etc. [2]. The prevalence of adrenal incidentaloma has been reported to be 1–6% [2]. The clinical questions for adrenal incidentaloma are whether it is functioning and whether it is malignant. A nationwide survey of adrenal incidentaloma in Japan revealed that 50.8% of total adrenal incidentalomas were non-functioning adenomas while 1.4% were adrenal cortical carcinomas [3]. We present a case of adrenal incidentaloma which was later found to be cavernous hemangioma of the adrenal gland in postoperative pathological examination.
Case Report
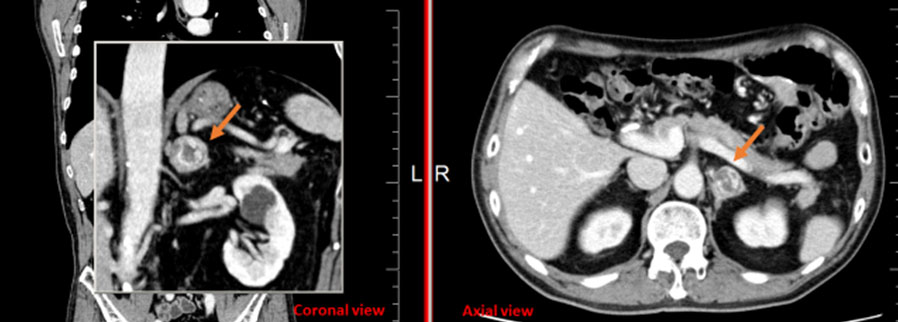
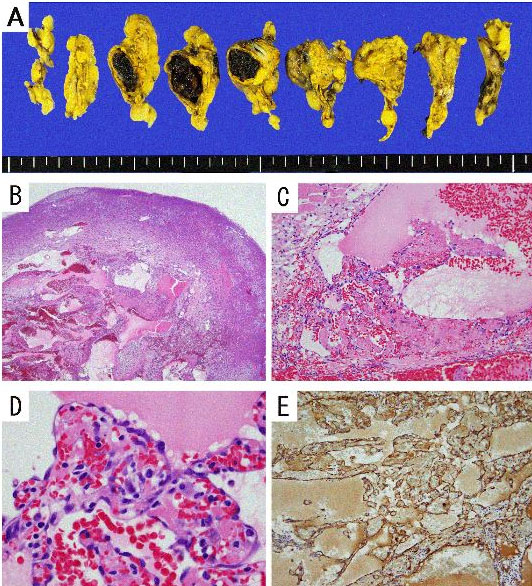
A 66-year-old Japanese man was hospitalized for the treatment of a left adrenal tumor. The tumor was first discovered incidentally in 2015 and had been followed up by computer tomography (CT). The patient had a past history of gastric cancer. The patient was followed for five years until 2020, when the size of the tumor had increased from 15 mm in length in July 2015 to 28 mm in July 2020 (Figure 1). The results of laboratory tests including hormonal values revealed no abnormality. A laparoscopic total adrenalectomy was performed on September 11, 2020. In gross findings, the tumor was 21 × 13 × 18 mm in size and contained some areas of necrosis and calcification (Figure 2A). The vascular tumor in medulla was observed in HE stain (Figure 2B). In microscopic findings, some irregular blood-filled vascular spaces with and endothelial lining were observed (Figure 2C). A papillary-expanding lesion of the mass was lined with a single layer of endothelial cells (Figure 2D). The immunohistochemical result was positive for blood coagulation factor VIII, demonstrating the tumor’s endothelial nature (Figure 2E). No evidence of malignancy was identified. The pathological diagnosis was cavernous hemangioma in the medulla of the left adrenal gland. There was no adverse event after the patient’s adrenalectomy, and there has been no evidence of recurrence since then.
Discussion
Hemangiomas are benign vascular tumors that probably arise from embryonic remains of unipotent angioblastic cells [4]. Histologically, adrenal hemangiomas are categorized into two groups: cavernous and capillary. Cavernous hemangioma of an adrenal gland is one of the rarest nonfunctioning tumors; <100 cases have been reported [1]. It might be encountered at the time of a pathology examination, and surgical intervention is sometimes necessary to rule out any malignant potential and lighten the secondary symptoms that have arisen due to the mass effect [5].
Cavernous hemangiomas of an adrenal gland involve the adrenal cortex and exhibit multiple dilated vascularity. The lesions are well-encapsulated and located in the adrenal cortex. They usually contain areas of hemorrhage, necrosis, degeneration, and calcification. Regarding clinical features, Noh et al. reviewed 52 cases of adrenal cavernous hemangiomas and reported that the median patient age at the time of diagnosis was 61.8 years; 33 patients (63.5%) were female; more than half of patients (53.8%) have no symptoms, and only three patients (5.8% of the cases) showed endocrine disturbances [6]. In our patient, neither symptoms nor laboratory abnormalities were present.
Concerning the CT findings, characteristic for adrenal hemangioma is the presence of both peripheral mottled pattern and afferent enhancements, heterogeneous internal structure, calcification, and highly enhanced rim on contrast CT [6],[7]. Benign mass has feature of mass without enhancement. Adenoma has smooth margin with homogeneous density <10 Hounsfield units (HU) on non-contrast CT [8]. Homogeneous adrenal density <10 HU with fat attenuating in the lesion may be a feature of myelolipomas [8]. Malignancy should be suspected for a mass with an irregular margin and heterogeneous density with a thick enhancing rim on contrast CT [9]. Adrenal mass with high enhancement may indicate the presence of pheochromocytoma and in that case, the use of either I131 metaiodobenzylguanidine (MIBG) or In111 octreotide may help for the diagnosis [8],[9].
In our patient’s case, the non-contrast CT showed a heterogeneous internal structure, and the contrast-enhanced CT revealed a supra-renal mass 2.8 cm in size with an enhanced capsule and a delayed enhanced mottled pattern core. The tumor margin was regularly enhanced. Calcification and heterogeneous enhancement due to necrosis were not observed on the CT images. Malignancy was thus unlikely in the qualitative diagnosis, but the increase in the tumor’s size could not rule out the possibility of malignancy.
Although magnetic resonance imaging (MRI) was not performed for this patient, a cavernous hemangioma’s appearance on MRI is characterized by a hypointense, heterogeneous lesion with a slightly hyperintense center on T1 images, and a high intensity peripheral rim on T2 images [10].
Conclusion
The preoperative diagnosis of cavernous hemangioma remains difficult because this tumor produces no particular clinical symptoms, laboratory results, or imaging findings. Resection is desirable because not only it is difficult to differentiate between cavernous hemangioma and adrenal tumor; there is also a risk of rupture or hemorrhage
REFERENCES
1.
Wang L, Dang Y, He R, Chen G. Rare cavernous hemangioma of adrenal gland: Case report. Sao Paulo Med J 2014;132(4):249–52. [CrossRef]
[Pubmed]

2.
Kebebew E. Adrenal incidentaloma. N Engl J Med 2021;384:1542–51. [CrossRef]
[Pubmed]

3.
Ichijo T, Ueshiba H, Nawata H, Yanase T. A nationwide survey of adrenal incidentalomas in Japan: The first report of clinical and epidemiological features. Endocr J 2020;67(2):141–52. [CrossRef]
[Pubmed]

4.
Jahn H, Nissen HM. Haemangioma of the urinary tract: Review of the literature. Br J Urol 1991;68(2):113–7. [CrossRef]
[Pubmed]

5.
Degheili JA, Abou Heidar NF, El-Moussawi M, Tawil A, Nasr RW. Adrenal cavernous hemangioma: A rarely perceived pathology—Case illustration and review of literature. Case Rep Pathol 2019;2019:8463890. [CrossRef]
[Pubmed]

6.
Noh J, Choi SH, Hwang HK, Kang CM, Lee WJ. Adrenal cavernous hemangioma: A case report with review of the literature. JOP 2014;15(3):254–7. [CrossRef]
[Pubmed]

7.
Sala S, Zatelli MC, Carcoforo P, Feo CF. Adrenal cavernous hemangioma: A case report. BMC Surg 2018;18(1):103. [CrossRef]
[Pubmed]

8.
Mayo-Smith WW, Song JH, Boland GL, et al. Management of incidental adrenal masses: A white paper of the ACR incidental findings committee. J Am Coll Radiol 2017;14(8):1038–44. [CrossRef]
[Pubmed]

9.
Farrugia FA, Misiakos E, Martikos G, et al. A step by step approach in differential diagnosing of adrenal incidentaloma. Rom J Intern Med 2017;55(4):188–97. [CrossRef]
[Pubmed]

10.
Edwards JP, Stuart HC, Urbanski SJ, Pasieka JL. A rare cavernous hemangioma of the adrenal gland. Int J Surg Case Rep 2014;5(2):52–5. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Acknowledgments
This work was supported by JSPS KAKENHI Grant Number 2OKO9548.
Author ContributionsTakashi Ando - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ei-Ichiro Takaoka - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Hiromu Inai - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Shinya Okada - Conception of the work, Design of the work, Acquisition of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Katsunori Uchida - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Jun Miyazaki - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2021 Takashi Ando et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.